What, dogs as cancer markers?
I first learned of the ability of dogs to sniff out cancers from a letter published in the prestigious Lancet. It cited a story of a woman whose dog constantly sniffed at a mole on her leg. On one occasion, the dog even tried to bite the lesion off. The constant attention from the dog prompted her to seek medical advice and when the path lab report came back, it was found to be a malignant melanoma!
Since it was caught early, the patient recovered fully from this very dangerous cancer and has remained well, with no sign of recurrence. The dog saved her life.
In another instance, a man aged 66 years developed a patch of eczema on the outer side of his left thigh, which grew slowly over 18 years, to about 1–2 cm in diameter. When dry, the lesion would become scabby, and it caused occasional itching. Various doctors tried treating it with steroids and antifungal creams, without any benefit.
Then a pet Labrador arrived in the home and the dog began to persistently push his nose against his owner’s trouser leg, sniffing the skin lesion beneath it. This prompted the patient to return to his family physician for review. An excision biopsy (removal) showed it to be a basal cell carcinoma. After it was gone, the dog showed no further interest in the area, so the animal was definitely reacting because of the pathology.1
Naturally, the idea of a pet detecting dangerous cancers and saving the owner’s life generated a lot of media interest. It makes sense: with about 220 million scent receptors (humans only have 5 million) dogs can be expected to smell things that could not possibly be detected by humans. Dogs have smell receptors 10,000 times more accurate than ours, which means their nose is powerful enough to detect substances at concentrations of one part per trillion – a single drop of liquid in 20 Olympic-size swimming pools!
Subsequently, a dermatologist in Florida teamed up with a retired police-dog handler with 33 years’ experience in training dogs, including service in Vietnam. They used conventional sniffer-dog techniques to train George, a schnauzer, to recognize pathological specimens of malignant melanoma and set him to work on humans.
George was introduced to a patient with several moles thought to be cancer-free. However one mole caused George to get very excited, and excision of the lesion confirmed early malignant disease.

So the idea of dogs being able to sniff out disease, often before any overt pathological changes have taken place, has begun to take hold of the medical community. They’ll be looking for ways to make money at it. But what the heck, if a few dogs acquire the skills, I foresee queues of worried people lined up outside the kennels for a walk past!
Better than oncologists by far!
Further investigation has showed that dogs are astonishingly accurate (far more accurate than oncologists with all their paraphernalia). Dogs were 97% successful at detecting lung cancer* and scored an impressive 88% at detecting breast cancer, regardless of attempts to mask the smell through food or cigarettes.
Other scientific studies have documented the abilities of dogs to identify chemicals that are diluted as low as parts per trillion.
Already dogs are used to warn of epileptic seizures, low blood sugar and heart attacks, although whether they are detecting changes in smell or physical behavior is still unknown. Some canines know how to call 911 in an emergency.
A 2006 study, led by Michael McCulloch of the Pine Street Foundation in San Anselmo, California, and Tadeusz Jezierski of the Polish Academy of Sciences, Institute of Genetics and Animal Breeding, investigated whether dogs could detect cancers only by sniffing the exhaled breath of cancer patients.2
In this study, five household dogs were trained within a short 3-week period to detect lung or breast cancer by sniffing the breath of cancer participants. The trial itself consisted of 86 cancer patients (55 with lung cancer and 31 with breast cancer) and a control sample of 83 healthy patients. All cancer patients had recently been diagnosed with cancer through biopsy-confirmed conventional methods such as a mammogram, or CAT scan and had not yet undergone any chemotherapy treatment.
During the study, the dogs were presented with breath samples from the cancer patients and the controls, captured in a special tube. The results of the study showed that dogs can detect breast and lung cancer with sensitivity and specificity between 88% and 97%.
The high accuracy persisted even after results were adjusted to take into account whether the lung cancer patients were currently smokers. Moreover, the study also confirmed that the trained dogs could even detect the early stages of lung cancer, as well as early breast cancer. The researchers concluded that breath analysis by trained dogs has the potential to provide a substantial reduction in the uncertainty currently seen in cancer diagnosis.
Breath Testing
The presence of chemicals in exhaled breath indicative of disease is itself nothing new. One of the critical tests for the presence of Helicobacter pylori, the stomach bug frequency associated with peptic ulcer (and therefore the “cause” of peptic ulcers to modern reductionist thinking), is the amount of hydrogen in exhaled breath from the patient.

In my book One Diet For Life I pointed out the value of this breath test in detecting dysbiosis. Inadequate digestion and malabsorption allows a test sugar load to reach the colon and there cause fermentation by bacteria.
Martin Gotteland and colleagues at the Institute of Nutrition and Food Technology in Santiago, Chile have shown conclusively that effective probiotic administration in humans significantly reduces hydrogen gas in excreted breath.
Where Next?
The next stage is to explore more fully the possible uses of dogs in early detection. Could dogs pick up Ebola, TB or AIDS in travelers returning from high risk areas? We don’t know. But we do know that a dog’s sense of smell is very complex and has “layers”, unlike our ability to focus on just one chemical at a time.
Since I originally wrote this article, canines proved to be able to correctly pick out the scent of a number of troubling conditions. For example, children infected with malaria parasites were correctly picked out 70 percent of the time, from socks they had worn all night!3
A study published in 2013, found that two trained dogs detected 11 out of 12 narcolepsy patients using sweat samples, demonstrating that dogs can detect a distinct scent for the disorder. The dogs pick up on biochemical changes in the body that lead to an attack and help with different tasks to avoid injury. But most importantly, they can provide a warning up to 5 minutes before an attack comes on, giving their handler a chance to get to a safe place or a safe position.4
A small 2019 study published in the prestigious Nature journal found that dogs were able to clearly discriminate a general epileptic “seizure odour.”5
The latest example of dogs detecting disease is with coronavirus SARS-CoV-2.
In a pilot study at the University of Helsinki, dogs were taught to recognize the previously unknown signature odor of COVID-19. And in only a few weeks, the first dogs were able to accurately distinguish urine samples from COVID-19 patients from urine samples of healthy individuals, almost as reliably as a standard PCR test.6
It is still unclear which substances in urine produce the apparently characteristic COVID-19 scent. Since SARS-CoV-2 not only attacks the lungs, but also causes damage to blood vessels, kidneys and other organs, it is assumed that the patients’ urine odor also changes. Researchers have high hopes it is the case since respiratory diseases like COVID-19 change our body scent, so there is a very high chance that dogs will be able to detect it.
Another project focused specifically on detecting ovarian cancer through analysis of exhaled breath has been awarded a federal research grant by the Congressionally Directed Medical Research Program. Epithelial ovarian cancer is the fifth leading cause of cancer death in women. Early diagnosis is the most important step toward reducing morbidity and mortality from epithelial ovarian cancer. If found early, even in the hands of conventional oncologists the (5-year) survival rate is over 90%.
The existing best current method to test for ovarian cancer, a combination of a blood marker called CA-125 and ultrasound of the lower abdomen, is really not an accurate indicator of early-stage disease.
Preliminary tests, under careful double-blinded conditions, showed the ability of trained dogs to distinguish ovarian cancer cases from controls using samples of exhaled breath condensate with accuracy of over 97%. Their hit rate was compared to that of a method involving a super-accurate instrument called a Gas Chromatography/Fourier transform Ion Cyclotron Resonance Mass Spectrometer (GC/FT-ICR MS). I have already explained the principle of cyclotron resonance in the book Medicine Beyond and predicted its growing place in modern medicine as a “virtual diagnostic” tool.7
Knowing more precisely what the dogs are noticing would allow their training to be standardized, but even then the skepticism of the medical community might prevail. Not all doctors would want to rely on a dog to make a diagnosis. Further studies may help convince reluctant doctors to use them as part of the preliminary screening process—but don’t hold your breath.
Of course if the relevant breath marker chemicals are identified, it may be possible to dispense with the doggies altogether.
But personally I think I’ll take the dog for a walk and if it yaps excitedly at a neighbor’s gate I might feel inclined to ring the bell and ask if everyone inside is OK!
To your good health,
The Official Alternative Doctor
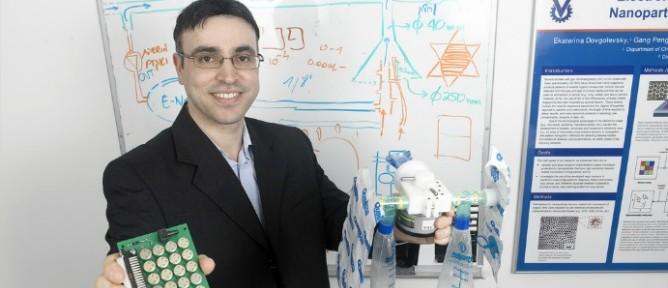
UPDATE: As I predicted in 2014, “Dr. Fido” is being challenged by a fake nose, the “Na-Nose” (nano nose, get it?) It was developed by a team of Israeli, American, and British cancer researchers and appears to have a high accuracy rate in detecting lung cancer, just by “sniff”. It can even identify what stage the cancer has progressed to.
The NaNose was able to detect lung cancer pretty well, even when the lung nodule was tiny and hard to sample. It was even able to discriminate between subtypes of cancer, which was unexpected.
Inventor and boffin Prof. Hossam Haick has been working on what he calls “Na-Nose” since 2007, and the device has been proven in numerous international clinical trials to differentiate between different types and classifications of cancer with up to 95 percent accuracy.8
Na-Nose’s detection device can be used at three different stages:
1. The first, and most critical, is advanced screening. The earlier cancer is detected, the better the survival rate.
2. The second stage is detailed diagnosis and monitoring during the cancer treatment: a simple breath analysis could mean less radiation or fewer biopsies.
3. And finally, the Na-Nose can be used following successful treatment, to stay on top of any signs that the cancer may be recurring.
References:
1. Williams H, Pembroke A. Sniffer dogs in the melanoma clinic?. Lancet 1989; 1: 734
2. McCulloch M., Jezierski T., Broffman M., Hubbard A., Turner K., Janecki T. 2006.Diagnostic accuracy of canine scent detection in early- and late-stage lung and breast cancers. Integrative Cancer Therapies 5, 1: 1-10.
3. https://www.wired.com/story/a-malaria-breathalyzer-its-closer-than-you-think/
4. Semergen. 2013 Oct;39(7):e41-6, 348-53. doi: 10.1016/j.semerg.2013.06.002. Epub 2013 Jul 5.
5. https://www.nature.com/articles/s41598-019-40721-4
6. https://www.helsinki.fi/en/news/healthier-world/finnish-covid-dogs-nose-knows
7. March 2006 issue of the Journal of Integrative Cancer Therapies published by SAGE Publications; European Lung Foundation, news release, Aug. 17, 2011.
8. Open Biomed Eng J. 2015 Aug 31;9:228–233. doi: 10.2174/1874120701509010228




