These antibiotics can’t be patented, are cheap, plentiful and are Nature’s blessed gifts to us. You can access them anywhere, except perhaps the darkest polar nights. Can you guess what they are?
Fresh air and sunshine.
You probably think I’m joking. But fresh air and sunlight are among the oldest concepts in medicine. Florence Nightingale famously promoted them. What’s more, they were effective.
She slashed hospital death rates with a host of hygiene improvements – including throwing open the windows. “It is necessary to renew the air round a sick person frequently, to carry off morbid effluvia from the lungs and skin,” she wrote.
But less well known is the fact that “Nightingale wards”, as they became known, had their long sides south-facing to let in plentiful sunlight.
Soon the health benefits of sunshine became more widely recognized, particularly for people with tuberculosis, which in Victorian times caused around one in five deaths in our crowded cities.
Sunlight not only kills airborne bacteria and those on the skin, but also seems to kill TB microbes inside the body, probably by boosting production of vitamin D, which has powerful effects on the immune system.
By the turn of the 19th century “solar clinics” were in vogue, utilizing fresh air and sunlight as part of TB treatment. Hospital beds were wheeled on to balconies or conservatories with special glazing that allowed ultraviolet light to pass through.
What Does Science Say?
Actually, there’s a very interesting report in this week’s New Scientist, about two experimenters at the Porton-Down defense facility in the UK (for those of you living outside the UK, this is a well-known bio-warfare site).
Microbiologists Henry Druett and K. R. May had speculated what would happen if deadly pathogens were exploded over a major city: how long would the microbes remain viable?1
To find out, they exposed E. coli to fresh air and were astonished that all viable microbes were dead within 2 hours, while controls kept in boxes at identical temperature and humidity largely survived.
So Florence Nightingale was right! Open windows not only diluted pathogens but actually destroyed them. The term “fresh air factor” was so named; it’s the newest-oldest antibiotic!
The sunlight is no mystery either. As I said, we know it boosts vitamin D levels and that will favor the immune system over invaders.
Trouble is, these cheap and effective remedies fell out of favor, due to the rise of antibiotics and their manifest success in conquering infections.
Moreover, in the 1970s, energy conservation became a big issue. Open windows and circulating air are the kiss of death to economic heating. Everything was sealed up. We entered the era of “sick building syndrome” (tight building syndrome in the USA).
Filtered air, it emerges, is deadly because it circulates pathogens in an unnatural and dangerous degree. As we get more and more crowded together in our cities and buildings, the dangers increase.
For instance, US soldiers stationed in the Saudi Arabian desert during the first Gulf war got more coughs and colds if they slept in air-conditioned barracks than if they bedded down in tents and warehouses.
Another study looking at Chinese college students found that 35 per cent of those who slept in poorly ventilated dorm rooms got an infection over the course of a year, compared with 5 per cent in rooms that were better ventilated.
That’s a 7-fold decrease in pathogenic activity. It’s time to go back to the old ways. They DID work, as I have explained.
Is There A Fresh Air Factor?
The answer is hydroxyl radicals. These short-lived molecules are constantly produced in the atmosphere through reactions between ozone and water, catalyzed by airborne organic chemicals from plants. They kill bacteria but are (relatively) harmless to humans.
But it’s also possible to produce them synthetically and I expect devices of this type will be widely available commercially, as the obvious failure of antibiotics looms larger and larger.
The Sunlight Factor
Science has the answer here too. We know that UV light is antiseptic. But it is also supposedly dangerous.
Drenching kids with UV light to boost their vitamin D levels was fashionable when I was a kid but soon went out of favor, as it was realized that UVB damages skin. Now we even worry about UVA.
But it has been found that the most useful wavelength is 207 nm. At this wavelength the UV is absorbed by protein molecules and therefore penetrates only a short way into human cells; it does not reach the DNA to cause mutations.
Microbes, on the other hand, are so much smaller than human cells that they completely absorb the light and are zapped. 
Now a lamp has been developed that emits only UV at 207 nm. Studies on cells grown in the lab have shown that this narrow band does not harm human skin tissue cultures yet kills bacteria, including MRSA.
Ive written about the use of UV technology (and plain blue light) in my block-buster compendium of alternative antibiotics.
You need to get it and read it. No use waiting till somebody is deadly ill. There are countless cases of people feeling a little ill at breakfast time and being dead before bedtime. That’s how fast bacteria multiply and do their deadly work.
The Bacteria Social Network
Also in my book “How To Survive In A World Without Antibiotics”, I explained what we call quorum sensing in bacteria. It’s like microbial Facebook!
When enough bacteria are present and “texting” each other, they reach a critical trigger point and suddenly explode as pathogens.
In the pipeline now are “quorum-blocking” drugs, which, rather than killing bacteria, merely stop them from mounting such an attack; it’s like shutting down their Facebook accounts. Importantly, such drugs are probably less likely to trigger resistance than conventional antibiotics.
Another option is phage therapies, using viruses genetically engineered to destroy bacteria. Here the New Scientist journalist and editor got it wrong. According to them, such a strategy is some years away from reaching the clinic.1
In fact, as I explain in my book, phage therapy is alive and well in the Eastern Bloc. Russia has a long and successful track record of using this kind of approach to microbes.
The drawback, as I explained, is that there is only one killer virus “phage” for any given pathogen. It will kill and eat its target bacteria all right, but there is no general phage to kill all or most pathogens, like penicillin does.
The Future
In the meantime, I think it pays to learn from the heroes of the past. Florence Nightingale slashed the death rate in the hospital of the Crimean War. Until she came along, soldiers were more likely to die of “hospital” than they were of dying of wounds on the battlefield!
It’s like today, when patients are very likely to catch a dangerous infection when they go to hospital. In the UK, 9% emerge with an infection they wouldn’t have caught elsewhere. In the USA, 100,000 a year die from such hospital infections.2
That’s three times the number that died of HIV.
The World Health Organization has published a report urging all healthcare settings to use natural ventilation as far as possible, even referencing Florence Nightingale.3 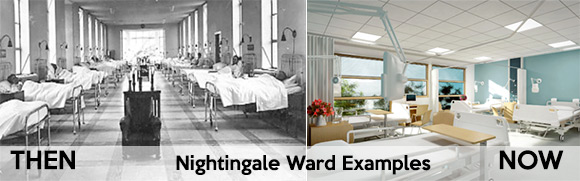
In Mumbai, India, an old-style sanatorium is being refitted as a clinic for people with drug-resistant TB, making use of an open-air regime.
It has high ceilings and open balconies. We seem to have come full circle in hospital design. Don’t miss out on the wealth of antibiotic alternatives available today.
Prof. Keith Scott-Mumby
