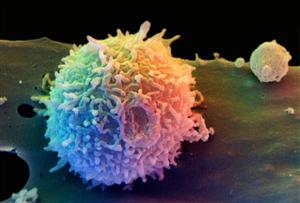
 When an infective organism invades the tissues, a precise series of events are set up to limit spread of the foreigner and ultimately to destroy it. First a macrophage will encounter the intruder. It engulfs it and then ‘displays’ its characteristic proteins on the surface of the cell as a kind of “flag” or gotcha trophy. We call this chemical flag the antigen, since it generates the rest of the reaction.
When an infective organism invades the tissues, a precise series of events are set up to limit spread of the foreigner and ultimately to destroy it. First a macrophage will encounter the intruder. It engulfs it and then ‘displays’ its characteristic proteins on the surface of the cell as a kind of “flag” or gotcha trophy. We call this chemical flag the antigen, since it generates the rest of the reaction.
By means of chemical language (a sort of local hormone called a lymphokine), the macrophage attracts nearby T-helper lymphocytes. They ‘read’ the antigenic matter and go off to program B-cells to produce antibodies to this pattern. The antibody is our own, the good guys’ response, to lock onto antigen carriers and cripple them.
T-helpers also secrete other lymphokines, which attracts further T-cells, killer cells and boosts the function of the B-cells, resulting in more antibodies against the invader.
Eventually, the enemy is overwhelmed by force majeur.
Two further steps are important. One is the introduction of memory T-cells. This really is the essence of lasting immunity; the cells learn to ‘remember’ the particular antigen involved. When a subsequent infection takes place, they can almost instantly mount the antibody response, without going through the above steps, because they remember the antigen and already have the antibodies ‘on tap’.
Finally, there must be some way of switching off the reaction. This is where the T-suppressor lymphocytes come in. They scale down the whole process and limit further response. Nature doesn’t want this destructive process to go on any longer than necessary.
It is a clever and spectacularly successful system, the detailed complexity of which surpasses our full understanding so far. The main drawback is that the body has to meet the foreign protein (antigen) before it can mobilize its counter-attack (the antibody). In other words, we must be invaded before we can fight back. This may not matter much with an illness like German measles or chicken-pox, but it is a serious inadequacy when it comes to potentially fatal diseases such as smallpox and diphtheria. Basically, those who survive such dangerous infections do so because their immune systems work very fast and start to produce antibodies in the nick of time, just before death supervenes. Those with a slower immune response are not so lucky and will die.
Or at least they used to. Now we can use vaccination to prevent such deaths. We introduce an artificial infection, commonly done by injecting a dead or weakened virus which does not harm the patient, but teaches his or her body to recognize the virus protein and make antibodies. Thus when the real invaders come along the body is ready and can start its counter-offensive by mobilizing antibodies within hours, instead of days, and so beat off the attack.
The frightening new disease AIDS (Acquired Immune Deficiency Syndrome) destroys T-lymphocytes and B-lymphocytes so that the body cannot make enough antibodies. The victim, therefore, dies of simple everyday infections which can no longer be resisted in the way in which a healthy individual routinely shrugs them off. Ironically, of course, it means also that the body is hampered in its ability to round on the AIDS virus and so this is a particularly grim infection. The search for a vaccine seems very bleak.
Other Cells which may be involved
The eosinophil is a cell mobilized especially against parasites and allergens. The monocyte is a short-lived circulating phagocyte that differentiates into the macrophage, a cell that may live from months to several years. The macrophages (literally “great gobbler” cells) are the sweep clean army of the immune system, engulfing bacteria, viruses, circulating cell debris and aggregations of immune complexes.
These cells tend to reside in various organ systems, where they selectively differentiate according to the needs of their host organ. For example, macrophages in the liver are celled Küpffer’s cells, and those in the lung are termed alveolar macrophages. The macrophage, like other phagocytes, depends on the generation of free radicals such as peroxide to destroy its target matter.
Mast cells are involved in the histamine response (redness, swelling and itching) that characterizes allergic reactions, such as dermatitis.
Click here to learn more about mast cells and histamine release.
Complement
The complement system is another immune response highway which helps to amplify the efficacy of immune reactions. “Complement” is actually a group of active enzymes which work in a cascade or tumbledown effect; the release of one triggers the next and so on, in sequential fashion. They are generally identified in the laboratory as C1 to C9.
The antigen-antibody complex combines with C1, which in turn acts on C2 and C4. This acts on C3 and son on, in what is called a cascade effect, each step leading to the next. The resultant enzymes act on the invader in a variety of ways and also participate in a local tissue reaction, familiar to us as inflammation. Although this is unpleasant and can be painful, it does serve a purpose in containing the attack.
Connect with us: Facebook – Twitter – LinkedIn – Google+ and take a look at our videos!
