If you turn to part 2 of my new book Virus Blitz! you’ll see that I have written a good deal about post-viral fatigue syndrome (PVFS), also sometimes called ME, and fibromyalgia (often confused with Lyme disease).
In that section I made a great issue out of the fact that—40 years ago—I was seeing people who seemed to be “allergic to exercise”, meaning they were made much worse by too much exertion.
There is no such thing as too much exertion, scoffed the experts. Nonsense; exercise more, they said! That’s the cure! One British doctor twerp said, “All these people need is anti-depressants and a good pair of running shoes.”
THIS WAS NONSENSE FROM IGNORANT BUT OPINIONATED IDIOTS.
I can confirm from my years of clinical experience with this condition that exertion was indeed the cause of much additional suffering. Markers of inflammation rose, symptoms worsened and patients—who were usually brave and endeavored to break out of their condition—would be put in their beds for several days on end.
It really was as if they were “allergic” to exercise.
Now the problem has surfaced again with investigations into long COVID (just another name for PVFS). People are being HURT because investigators are forcing them to exert themselves and not accepting that this is a grave problem, making patients WORSE.
See, I was right all along!
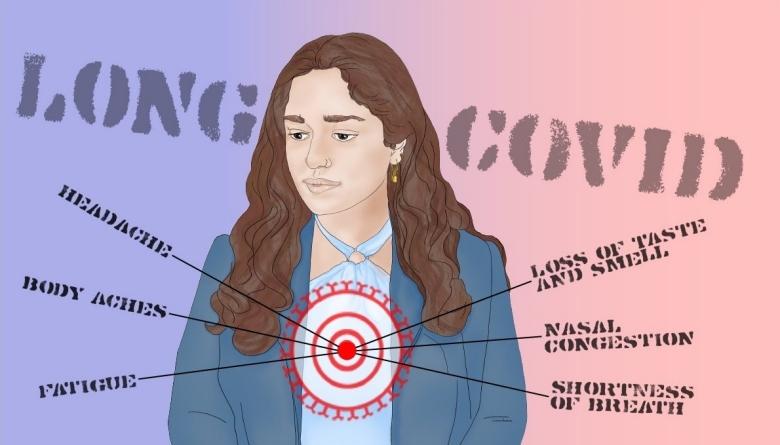
Patients and patient advocates are calling on the US National Institutes of Health (NIH) to reconsider its decision to include exercise trials in its RECOVER initiative (Researching COVID to Enhance Recovery), which aims to study and find treatments for long COVID. They argue that a large proportion of people with long COVID have reported experiencing post-exertional malaise (PEM) — a worsening of symptoms such as fatigue, difficulty regulating body temperature and cognitive dysfunction, after even light exercise — and worry that putting certain RECOVER participants through exercise trials could cause them harm.
Long-COVID Treatments: Why The World Is Still Waiting
Large numbers (many millions) of people worldwide have developed long COVID. The condition has affected their lives and livelihood: nearly 20% of them had still not returned to work more than a year after being infected with the coronavirus SARS-CoV-2. Advocates want to see the RECOVER exercise protocols because they are concerned that trial participants will not be adequately informed about the potential risks; that participants will not be properly screened for PVFS/PEM; and that researchers will not sufficiently monitor people for harm in the hours after the exercise regimen or after the trial concludes.
“In a world where there’s hundreds of things to trial, why are we choosing this one thing that we know has the potential to cause harm to a substantial portion of patients?” asks Lisa McCorkell, a co-founder of the Patient-Led Research Collaborative for long COVID, a research and advocacy group based in Washington DC.
GOOD question, Lisa. The answer is mainly stupidity, arrogance and lack of compassion, with more than a little ignorance thrown in, as an excuse!
The RECOVER Clinical Trials Center at the Duke Clinical Research Institute in Durham, North Carolina, is keeping its cards close to its chest.
Hitting A Wall
Journalist Jaime Seltzer, who has ME/CFS, experiences post-exertional malaise herself, comments:
“Long COVID isn’t the first disease for which people have reported experiencing PEM. People who have myalgic encephalomyelitis, also known as chronic fatigue syndrome (ME/CFS), have long reported exacerbation of symptoms after overexertion that make their day-to-day functioning difficult. Similar to long COVID, ME/CFS often develops after a viral illness; its symptoms include PEM, cognitive impairment and joint and muscle pain.”
Jaime first experienced PEM after some gentle exercise. “It felt fine until I hit my wall, after which I experienced a drop in core body temperature, started shaking, had trouble thinking,” says Seltzer, who is scientific and medical outreach director for the international advocacy organization #MEAction USA, based in Santa Monica, California, which sent the letters to the NIH. “It was like I had suddenly been dropped in the Arctic.” She then slept for 18 hours, after which she was unable to get out of bed.
Now people are hesitating about having kids because of the exertion involved. It’s hard enough bringing up kids, as every parent knows. But you just can’t do it with PVFS!
Time carries a story of a woman who was planning to have her eggs frozen and stored at age 30 years, so she and her partner could have a child when they felt ready.
Now she is so severely debilitated by the intense fatigue of long COVID, it makes it virtually impossible to exercise without crashing and feeling faint afterwards. At hercurrent energy levels, she says it’s hard to imagine caring for a pet, let alone a child.
[https://time.com/6268429/long-covid-reproductive-health/
Exercise Overload
As researchers find out more about long COVID, it has become clear that many people with the condition meet the criteria for ME/CFS. In a study published online late last year, researchers reported that of the 465 people with long COVID surveyed, 58% could be categorized as having ME/CFS.
And in a 2021 study, researchers at the Patient-Led Research Collaborative, including McCorkell, surveyed 3,762 people with long COVID and found that, over a 7-month period, one of the most frequent symptoms reported was PEM. Around 89% of participants reported experiencing PEM at some point during the course of their illness, with 72% of them still reporting it at month 7.
At last, they are getting it. But unfortunately, not everyone.
According to the NIH, RECOVER is the most ambitious long-COVID study yet, with the trials expected to last four years, and to enrol more than 15,000 adults and 6,000 children. All of this has advocates concerned about the inclusion of exercise trials in the RECOVER initiative.
“It is evident the NIH RECOVER initiative is made up of many folks who are dedicated and determined to crack open effective treatments for long COVID,” says Charles McCone, an advocate based in San Francisco who Nature identified as a patient representative for the RECOVER trial. But it is “baffling and discouraging” that the initiative is including exercise — a treatment that has ALREADY been shown to be largely ineffective and often harmful for those with ME/CFS, he says.

It seems that for many patients, Long COVID is more than a medical issue. It also affects work, relationships, and life plans—including when, how, and whether to have children.
What To Do
No doubt the reader will want to know what I worked out as the best approach to relieving PVFS/ME/now long COVID?
Well, that would be next week!
To your good health,
Prof. Keith Scott-Mumby
The Official Alternative Doctor
SOURCES: